PERSONA
Ana Nery - A Matriarca da Enfermagem no Brasil
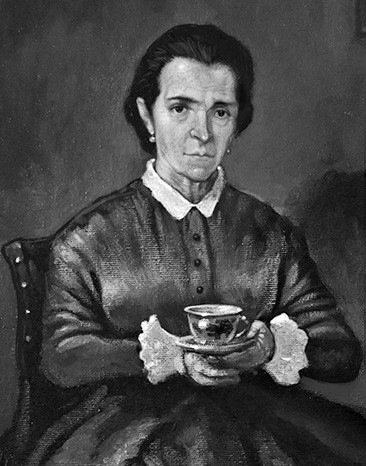
A primeira escola oficial de enfermagem de alto padrão no Brasil, fundada por Carlos Chagas em 1923, recebeu em 1926 o nome de "Ana Néri", em homenagem à primeira enfermeira brasileira, que serviu como voluntária na guerra do Paraguai. Ana Justina Ferreira Néri nasceu na vila de Cachoeira de Paraguaçu-BA, em 13 de Dezembro de 1814.
Viúva do capitão-de-fragata Isidoro Antônio Néri, viu seus filhos, o cadete Pedro Antônio Néri e os médicos Isidora Antônio Néri Filho e Justiniano de Castro Rebelo; seus irmãos Manuel Jerônimo Ferreira e Joaquim Maurício Ferreira, ambos oficiais do exército, serem convocados para a Guerra do Paraguai.
Ana Néri escreveu então ao presidente da província uma carta em que oferecia seus serviços como enfermeira enquanto durasse o conflito.
Partiu da Bahia, de onde nunca saíra, em 1865, para auxiliar o corpo de saúde do Exército, que era pequeno e contava com pouco material. Começou seu trabalho no hospital de Corrientes, onde havia, nessa época, cerca de seis mil soldados internados e algumas poucas freiras vicentinas. Mais tarde, assistiu os feridos em Salto, Humaitá, Curupaiti e Assunção.
Mulher de posses, com seus recursos montou na capital conquistada, na própria casa onde morava, uma enfermaria limpa e modelar. Ali trabalhou abnegadamente, até o fim da guerra, na qual perdeu seu filho Justiniano e um sobrinho, que se alistara como voluntário da pátria.
De volta ao Brasil, em 1870, Ana Néri recebeu várias homenagens: foi condecorada com as medalhas de prata humanitária e da campanha e recebeu do imperador uma pensão vitalícia, com a qual educou quatro órfãos que recolhera no Paraguai. Seu retrato de corpo inteiro, obra de Vítor Meireles, figura em lugar de honra no paço municipal de Salvador. Ana Néri morreu no Rio de Janeiro, no dia 20 de Maio de 1880.
Fonte: Secretaria do Estado de São Paulo
Florence Nightingale
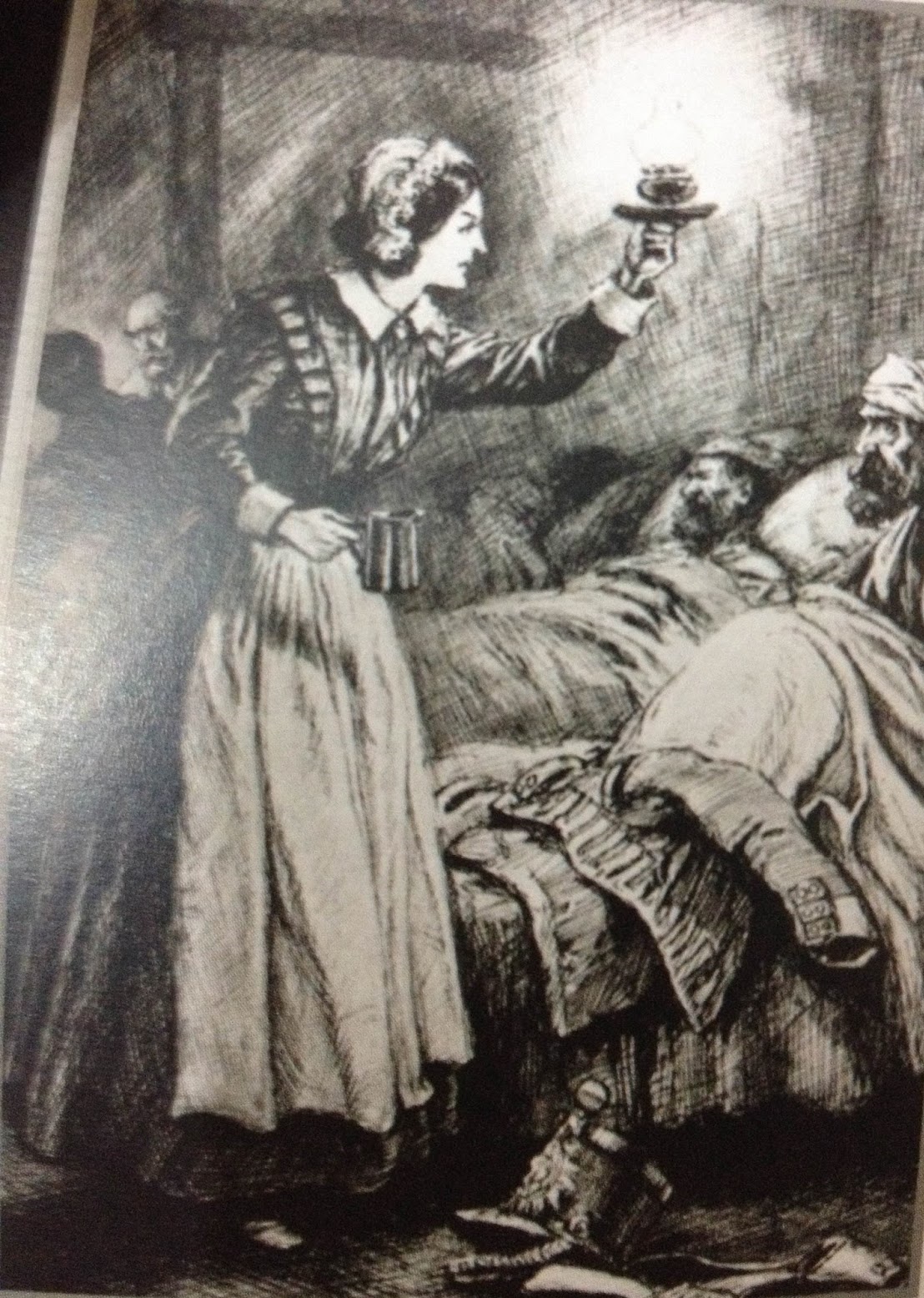
Florence Nightgale nasceu na Itália em 12 de maio de 1820, 2ª filha de uma família aristocrática européia. Sua família, rica e bem-relacionada, vivia em Florença na Itália. Por isso, Florence recebeu o nome em inglês da cidade em que nasceu, como sua irmã mais velha Parthenope nascida em Partênope. Moça brilhante e impetuosa, rebelou-se contra o papel convencional para as mulheres de seu status, que seria tornar-se esposa submissa, e decidiu dedicar-se à enfermagem. Foi uma enfermeira britânica que ficou famosa por ser pioneira no tratamento a feridos de guerra, durante a Guerra da Criméia. Também contribuiu no campo da Estatística, nomeadamente na criação de sistemas de representação gráfica como o gráfico setorial ("pizza") e para Controlde de Infecção, os princípios de Isolamentos para Doenças Infecciosas; de Higiene Pessoal e Ambiental; Lavanderia e Nutrição e Dietética.
Florence sofria de esquizofrenia. Em dezembro de 1844, em resposta à morte de um mendigo
numa enfermaria em Londres, que acabou evoluindo para escândalo público, ela se tornou a principal defensora de melhorias no tratamento médico. Imediatamente, ela obteve o apoio de Charles Villiers, presidente do Poor Law Board (Comitê de Lei para os Pobres). Isto a levou a ter papel ativo na reforma das Leis dos Pobres, estendendo o papel do Estado para muito além do fornecimento de tratamento médico. Ela anunciou sua decisão em torna-se enfermeira, papel exercido na época por mulheres ajudantes do hospital ou cozinheiras do exército, o que para a família em 1845, provocou raiva e rompimento, particularmente de sua mãe.
Em 1846, ela visitou Kaiserwerth, um hospital pioneiro fundado e dirigido por uma ordem de freiras católicas na Alemanha, ficando impressionada pela qualidade do tratamento médico e pelo comprometimento e práticas das freiras.
A contribuição mais famosa de Florence foi durante a Guerra da Criméia, que se tornou seu principal foco quando relatos de guerra começaram a chegar à Inglaterra relatando as condições precárias dos feridos. Em outubro de 1854, Florence e uma equipe de 38 enfermeiras voluntárias treinadas por ela, inclusive sua tia Mai Smith, partiram para a Criméia. Florence Nightingale voltou para a Inglaterra como heroína em agosto de 1857 e era provavelmente a pessoa mais famosa da Era Vitoriana além da própria Rainha Vitória.
Em 1860, estabeleceu a escola de treinamento para enfermeiras no hospital St Thoma´s, considerando a enfermagem como profissão respeitável para mulheres.
No mesmo ano, Florence publicou seu primeiro manuscrito com os princípios dos cuidados baseados na observação e sensibilidade às necessidades do paciente. As notas foram traduzidas para onze línguas estrangeiras e são publicadas até os dias atuais. Para Saúde Pública, o planejamento e organização do hospital tiveram um impacto profundo na Inglaterra e através do mundo. Fez campanha ao longo dos anos para melhoria dos padrões da saúde, publicando 200 livros, relatórios e panfletos.
Em 1883, a Rainha Vitória concedeu a Florence Nightingale a Cruz Vermelha Real e em 1907 ela se tornou a primeira mulher a receber a Ordem do Mérito. Florence não conseguia levantar da cama a partir de 1896 e morreu em 13 de agosto de 1910.
Florence Nightgale influenciou a natureza do cuidado de saúde moderno e seus manuscritos são referenciais atuais para a Enfermagem.
Fonte: Florence Nightingale Museum, London
Como Homenagem inicial deste SITE queremos referenciar O Prof. Dr. E. Donnall Thomas, idealizador do Transplante de Medula Óssea e premio Nobel em fisiologia em Medicina em 1990.
Dr. Edward Donnall Thomas was born in 1870 and moved to Texas with his family in a covered wagon in 1874. He grew up in frontier Texas and, with almost no formal schooling went to the University of Louisville, Kentucky, where he received his M. D. His first wife died of tuberculosis, and I was the only child of his second wife. He was 50 years old when I was born on March 15, 1920. He was a solo general practitioner in our small Texas village. Thus, together we span the time from horse and buggy house calls to modern high-tech medicine.
My high school class consisted of about 15 people. I was not an outstanding student even in this small group. I entered the University of Texas in Austin in 1937. In my first semester I made only B grades, but as time went on and the courses became more difficult and challenging I began to enjoy the studies, mainly in chemistry and chemical engineering. I received a B. A. in 1941 and an M. A. in 1943.
During my undergraduate years at the end of the depression money was almost non-existent so I worked at a number of odd jobs. One of the jobs was waiting tables at a girls' dormitory. One January morning it snowed, a rare event in Texas. As I emerged from the girls' dormitory, an attractive young woman hit me in the face with a snow ball. I naturally had to catch her and avenge the insult to my male ego. Thus, I meet Dorothy Martin, the Dottie who has participated in all my endeavors up to the present time. We have 3 children, Don Jr. who practices internal medicine in Montana, Jeffrey who is in business in Seattle and Elaine who is a Fellow in infectious diseases at the University of Washington. We have eight grandchildren.
I entered Harvard Medical School in 1943. During medical school Dottie abandoned her journalism work to enter training as a laboratory technician while working to help support us. Her training in writing, laboratory technology and library science has been invaluable in our work. I received the M. D. in 1946.
There followed an internship, a year of hematology training under my life-long friend Dr. Clement Finch, two years in the army, a year of postdoctoral work at Massachusetts Institute of Technology, two years of medical residency, the last as the chief medical resident at the Peter Bent Brigham Hospital in Boston. During that time Dr. Joseph Murray was a surgical resident and we have been friends and colleagues over the years because of our common interests in transplantation. I was on the wards of the Brigham and helped care for his first kidney transplant patient.
During medical school I became interested in the bone marrow and in leukemia. This interest was intensified by my early association with Dr. Sydney Farber who gave me my first laboratory in the new Jimmy Fund Building. I was fortunate to see the first child with acute lymphoblastic leukemia (ALL) whose remission was induced with an anti-folate drug. I became interested in factors that stimulate marrow function in part due to Allan Erslev's attempt to demonstrate erythropoietin. During my year at M.I.T. I worked under Dr. John Loofborrow on stimulating factors released from irradiated yeast. I hoped to apply this knowledge to marrow stimulating factors. Fortunately I left the field of stimulating factors because it is only in recent years, with recombinant technology, that great strides have been made in this area.
I had been intrigued by the studies of Dr. Leon Jacobsen et al. who demonstrated that shielding the spleen would protect mice against otherwise lethal irradiation and the subsequent demonstration by Egon Lorenz et al. that a marrow infusion was also protective. These observations were initially thought to be the result of stimulating factors. In 1955, Main and Prehn published their paper showing that a mouse protected against lethal irradiation by a marrow infusion would accept a skin graft from the marrow donor. Their study and the demonstration by Ford et al. using cytogenetic technology of donor chromosomes in such mice made it suddenly clear that the irradiation protection effect was due to the survival of living bone marrow cells.
In 1955, at the invitation of Dr. Joseph Ferrebee I went to the Mary Imogene Basset Hospital in Cooperstown, N. Y., an affiliate of Columbia University. Immediately, we began to work on marrow transplantation in human patients and in the dog, as an outbred animal suitable for clinical care comparable to human patients. Except for an occasional patient with an identical twin, we quickly learned that allogeneic marrow transplants in man were going to be very difficult. Joe Ferrebee and I and our young colleagues concentrated on working with our dogs on many aspects of marrow transplantation. The long cold winters, absence of commuting problems and opportunity for long discussions were conducive to our work. Those years had a deep and abiding influence on subsequent work since most of the basic concepts were laid out during that time.
In 1963 I moved to Seattle at the invitation of Dr. Robert Williams, a famous endocrinologist and first chairman of the Department of Medicine at the University of Washington. Professor Williams recognized that our School of Medicine was in its infancy and rather isolated in the Pacific Northwest. He envisioned the affiliation of all the relevant institutions in the area with the School of Medicine in order to create the critical mass necessary for academic excellence. Within that concept I established my program in the Seattle Public Health Hospital.
The rest of the story seems short in retrospect. The recruitment of some brilliant young co-workers who still work with me, studies of immunology and irradiation biology in the dog, borrowing knowledge of human histocompatibility from Amos, Payne and Dausset, the assembly and training of a critical care team of nurses, and, finally, the demonstration that some patients with advanced leukemia, aplastic anemia or genetic diseases could be cured by marrow transplantation.
Our team of physicians and nurses proved to be stable and dedicated. We did face problems that at times seemed almost insurmountable. In 1972, the Seattle Public Health Hospital was faced with closure by the federal government. After many conferences with the Dean of the School of Medicine, it was apparent that we could not move to the University of Washington. We found temporary space at Providence Hospital for a two year period. In 1975 our team moved into the Fred Hutchinson Cancer Research Center which provided superb facilities and the opportunity to expand the program with the cooperation of the Swedish Hospital Medical Center. While continuing laboratory and animal research, our team has now carried out more than 4,000 human marrow transplants.
It is always diffcult to identify the many threads that make up the fabric of a life's work. I know that my philosophy and ideas have been heavily influenced by more than 20 years of daily interaction with a small group of colleagues, all of whom are now distinguished scientists in their own right. Bob Epstein, Rainer Storb, Dean Buckner, Reg Clift, Paul Neiman and Alex Fefer were with me at the start of the Seattle adventure, and all except Bob are still my daily companions. Ted Graham moved with me from Cooperstown and has played an essential role in our animal research. Along the way we were joined by Joel Meyers, Fred Appelbaum, John Hansen and many others who made major contributions to the achievements honored by this award.
From Les Prix Nobel. The Nobel Prizes 1990, Editor Tore Frängsmyr, [Nobel Foundation], Stockholm, 1991 This autobiography/biography was written at the time of the award and later published in the book series Les Prix Nobel/Nobel Lectures. The information is sometimes updated with an addendum submitted by the Laureate. To cite this document, always state the source as shown above.
Fonte: www.nobelprize.org © The Nobel Foundation
npk gübre


